From Waste to Walking: Reusing Prosthetics Changes Lives Globally
From Waste to Walking: Reusing Prosthetics Changes Lives Globally
From Waste to Walking: Reusing Prosthetics Changes Lives Globally
-

-
Penta Medical Recycling has carved a special niche in global health by addressing the pressing needs of underserved amputees worldwide. This US nonprofit organization collects, refurbishes, and redistributes prosthetic components from across the United States to low- and middle-income countries, where resources are scarce and prosthetic care is often unaffordable. Over the eight years since its inception, Penta has expanded its operations to 29 countries across six regions of the world. Through a commitment to sustainability, innovation, and equity, Penta Medical Recycling exemplifies how the principles of the circular economy can be applied to transform lives.
Sustainability in prosthetic care: reusing and redistributing
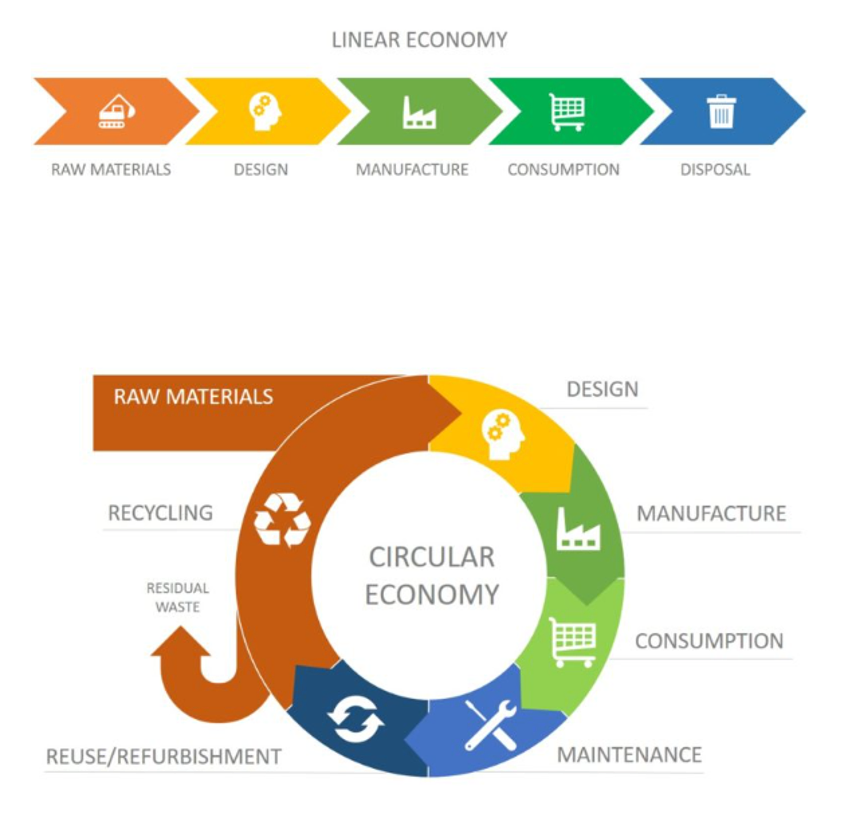
At the heart of Penta’s mission lies the principle of the circular economy: reusing and redistributing prosthetic components to reduce waste and maximize impact. By collecting used and new prosthetic parts from individuals and medical clinics in the US, the organization diverts these items from landfills and repurposes them for patients in need.
From an environmental standpoint, this approach tackles the significant issue of prosthetic material disposal. By diverting prosthetics from landfills through redistribution, the organization prevents these components from contributing to environmental pollution. Each reused component reduces the need for new manufacturing, saving valuable resources such as metals and polymers and mitigating the broader ecological impact of industrial waste.

Economically, this model alleviates financial burdens for both the organization and the recipients. Many prosthetic components—though no longer suitable for their original users—retain functionality. By redistributing these components, Penta Medical Recycling reduces the costs associated with creating new prosthetics and ensures that every dollar spent by donors has a greater impact.
On the social front, this sustainable model fosters inclusivity, giving amputees in underserved regions access to life-changing technology they would otherwise be unable to afford. It also helps address the inequities exacerbated by poverty, and systemic healthcare disparities.
Operational excellence: The inventory management system
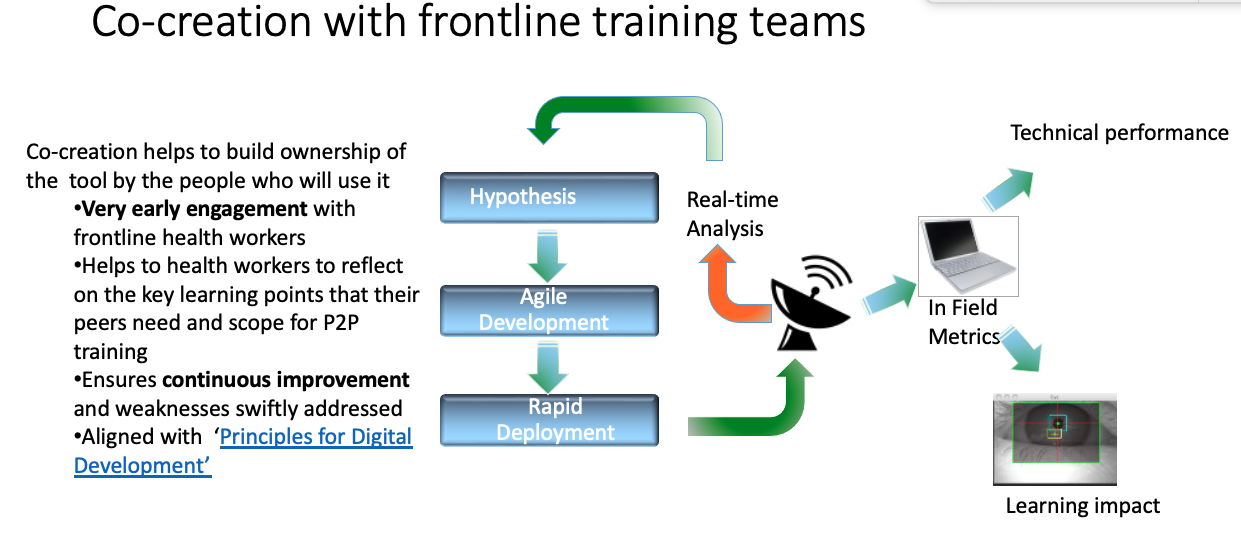
To ensure that these efforts are as efficient and impactful as possible, Penta developed a custom-built inventory management system. This system tracks each donated component from its arrival at the warehouse to its final placement with a medical centre.
The platform integrates live data, enabling partner clinics to view available inventory and request specific components in real-time. This outward-facing feature is key, as it empowers healthcare centres to directly choose prosthetics tailored to their specific needs. By allowing practitioners to match components with patient requirements, the system ensures prosthetists can select components that optimize the customization and fitting process.
“We believe in empowering healthcare centres. By allowing them to choose exactly what they need, we minimize waste and maximize patient outcomes.”
— Mija Strong, Director of Operations at Penta Medical Recycling

Vetting healthcare centres for equity
A cornerstone of Penta’s mission is ensuring that its resources reach those most in need. This commitment begins with a thorough vetting process for healthcare centres receiving prosthetic components.
Partners are evaluated based on their ability to provide equitable care and their adherence to ethical standards. Penta prioritizes clinics serving underserved populations, particularly those unable to afford prosthetic care independently. Conversations, site visits, and trial shipments form the foundation of these partnerships, ensuring that clinics can responsibly utilize the donated components.
Trust and accountability are reinforced through patient surveys and usage reports, which help track the impact of the distributed components. This approach mitigates risks, such as the misuse or resale of prosthetic parts, and ensures that the organization’s efforts align with its core mission.
Social impact and patient outcomes
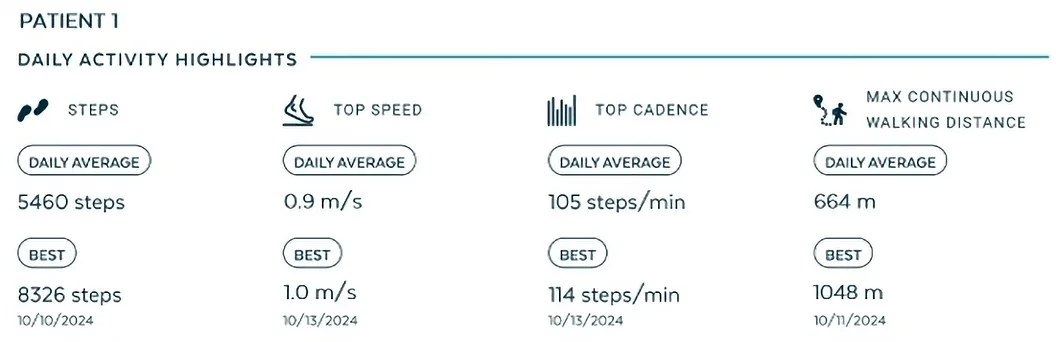
In 2024 alone, Penta distributed nearly 3,700 prosthetic components, enough to support at least 740 individuals. These numbers, however, tell only part of the story. Behind every shipment is a human narrative of restored mobility, independence, and dignity.
One instance involved a young donor in Philadelphia whose prosthetic components were refurbished and distributed to a boy in Liberia. The two later connected via a video call and were able to share the deeply personal impact on both. Such stories underscore the profound social value of Penta Prosthetics’ mission.
“Behind every shipment, there’s a story of renewed hope and mobility. This is why we do what we do.”
— Anna Szczepanek, Executive Director of Penta Medical Recycling
While collecting patient feedback is challenging, particularly in regions with limited healthcare infrastructure, the organization’s efforts to gather qualitative and quantitative data have improved over time. These insights not only validate the organization’s impact but also drive further support from donors and partners.

Nonprofit funding model
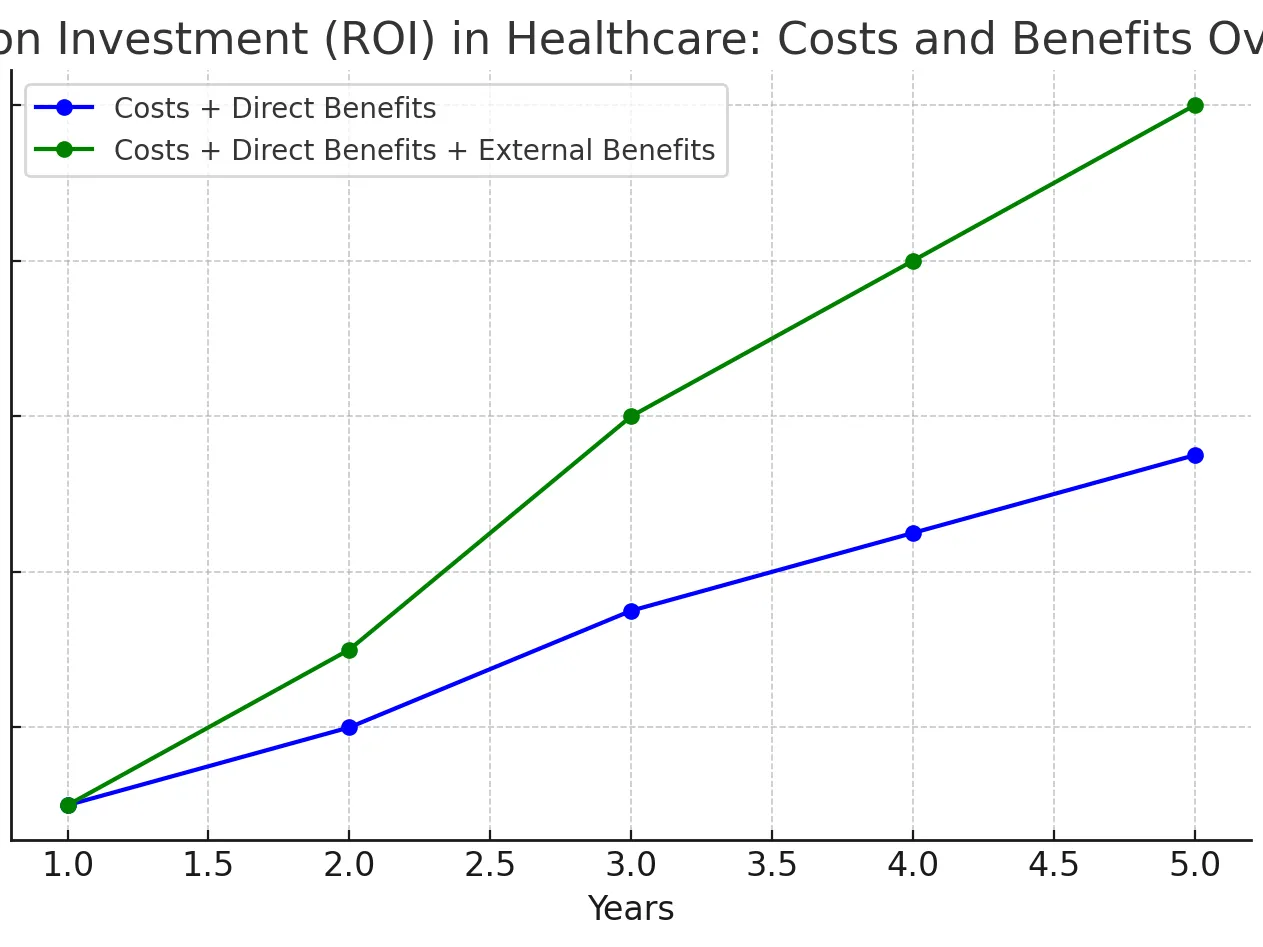
Penta operates as a nonprofit organization, relying on a diverse array of funding sources, including individual donors, family foundations, and grants. Despite its lean operations, the organization’s ability to sustain its mission hinges on consistent financial support.
One of the challenges lies in balancing operational costs, such as inventory management, with the need to expand services. To address these constraints, Penta Prosthetics has explored partnerships with corporate donors and other philanthropic entities. Additionally, its meticulous and transparent tracking system of every component strengthens donor trust, as donors of prosthetics can see the specific impact of their contributions.
“Through our system, a donor can track their knee going to Honduras and their pylon to Liberia, knowing exactly how each piece is giving someone a second chance at mobility.”
— Anna Szczepanek, Executive Director of Penta Medical Recycling
Conclusion
Penta Prosthetics is a testament to the transformative power of sustainability and innovation in global health. By integrating the principles of the circular economy into its operations, the organization reduces environmental impact, optimizes economic resources, and fosters social equity. Its cutting-edge inventory management system and rigorous vetting process ensure that its resources reach those most in need, amplifying its impact.
As Penta continues to grow, its mission remains clear: to restore mobility, dignity, and hope to underserved amputees worldwide. Through its commitment to sustainability, this small but deeply inspiring nonprofit offers a model for how compassion and ingenuity can create a more equitable world.