The importance of an evidence-based approach
Improved patient outcomes are a cornerstone benefit of evidence-based, data-driven healthcare. When medical decisions are grounded in rigorous scientific evidence and comprehensive data analysis, healthcare providers can significantly enhance their ability to diagnose, treat, and manage patient conditions. This approach allows for more accurate identification of diseases, selection of the most effective treatments, and better prediction of patient responses to interventions. By leveraging data from large-scale clinical trials, meta-analyses, and real-world evidence, clinicians can make informed decisions that are more likely to result in positive outcomes for their patients.
Reducing errors and risks is another critical advantage of data-driven healthcare. By systematically analysing large datasets, healthcare systems can identify patterns and correlations that may not be apparent in individual cases. This helps in recognizing potential risks, side effects, and contraindications associated with various treatments or procedures. For instance, data analysis can reveal unexpected drug interactions or highlight patient populations at higher risk for certain complications. By incorporating these insights into clinical decision-making processes, healthcare providers can significantly improve patient safety and reduce the incidence of medical errors.
Cost-effectiveness is a key consideration in modern healthcare systems, and evidence-based approaches play a crucial role in optimizing resource allocation. By focusing on treatments and interventions that have been proven effective through rigorous studies and data analysis, healthcare systems can avoid wasting resources on ineffective or unnecessary procedures. This not only reduces overall healthcare costs but also ensures that patients receive the most beneficial care. Evidence-based guidelines can help standardize care practices, reducing variability and associated costs while improving overall quality of care.
Personalized medicine represents a significant advancement enabled by data-driven healthcare. The analysis of large datasets, including genetic information, biomarkers, and patient histories, allows for the development of more tailored treatment approaches. This personalization takes into account individual patient characteristics, genetic predispositions, and specific circumstances to create targeted intervention strategies. By moving away from one-size-fits-all approaches, personalized medicine can improve treatment efficacy, reduce side effects, and enhance patient outcomes across a wide range of conditions.
Continuous improvement is an inherent feature of evidence-based healthcare. The ongoing collection and analysis of data enable the healthcare industry to identify trends, refine practices, and develop new treatments over time. This iterative process allows for the rapid incorporation of new evidence into clinical practice, ensuring that healthcare delivery remains current and effective. It also facilitates the identification of gaps in knowledge or areas requiring further research, driving innovation and advancement in medical science.
The prosthetics industry has faced several unique challenges in adopting a more data-driven approach to innovation, despite the clear benefits of evidence-based practices in healthcare. These barriers have contributed to the relatively slower pace of radical change in this sector.
What are the hurdles that have held the sector back?
There are many reasons why research and development in the field of prosthetics has struggled to realise the potential opportunity of data driven research.
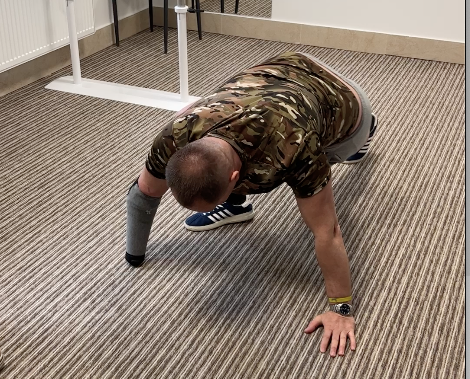
Limited data availability: The prosthetics field often deals with smaller patient populations compared to other medical areas. This can result in smaller datasets, making it more challenging to draw statistically significant conclusions or identify meaningful patterns. The highly individualized nature of prosthetic fittings and usage also complicates data standardization and aggregation.

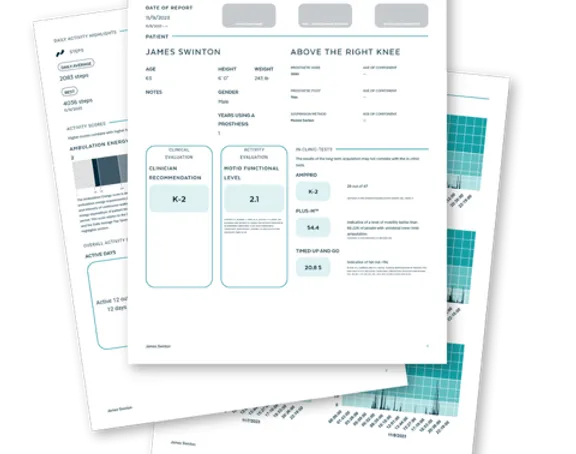
Complexity of outcome measures: Quantifying the success of a prosthetic device is multifaceted, involving factors such as functionality, comfort, aesthetics, and user satisfaction. This complexity makes it difficult to establish standardized outcome measures across diverse user populations, hindering large-scale data analysis and comparison of different prosthetic solutions.
Technological limitations: Until recently, many prosthetic devices lacked the capability to collect real-time usage data. The integration of sensors and data collection systems into prosthetics is a relatively new development, limiting the historical data available for analysis.

Privacy and ethical concerns: The collection of detailed, personal data about prosthetic usage and user behaviour raises significant privacy issues. These concerns can make users hesitant to share data and complicate the process of obtaining informed consent for data collection and analysis.
Fragmented ecosystem: The prosthetics industry involves multiple stakeholders, including manufacturers, clinicians, researchers, and users. This fragmentation can lead to data silos and challenges in data sharing and integration, limiting the potential for comprehensive data analysis.
Funding constraints: Research and development in prosthetics often receive less funding compared to more prevalent medical conditions. This limitation can restrict the resources available for implementing sophisticated data collection and analysis systems.
Regulatory hurdles: Stringent regulatory requirements for medical devices can slow down the implementation of new data collection technologies in prosthetics. Concerns about data security and the potential for data-driven features to be classified as medical interventions may further complicate regulatory approval processes.
Resistance to change: Traditional practices in prosthetics fitting and design have been based largely on clinical experience and craftsmanship. There may be resistance from some practitioners to shift towards more data-driven approaches, particularly if they perceive these methods as challenging their expertise or potentially reducing the personalized nature of their work.
Lack of standardization: The highly customized nature of prosthetics has led to a lack of standardization in design, components, and fitting procedures. This variability makes it challenging to compare data across different devices and users, complicating large-scale data analysis. Also, presenting data in a meaningful way that can be translated into specific actions can be challenging.
Technical expertise gap: Effectively implementing data-driven approaches requires expertise in data science, machine learning, and advanced analytics. There may be a shortage of professionals with both this technical knowledge and a deep understanding of prosthetics, limiting the industry’s capacity to fully leverage data-driven innovations.
Addressing these barriers will be crucial for the prosthetics industry to more fully embrace data-driven innovation. As technology advances and the benefits of evidence-based approaches become more apparent, we can expect to see increased efforts to overcome these challenges and accelerate progress in the field.
Looking to the future
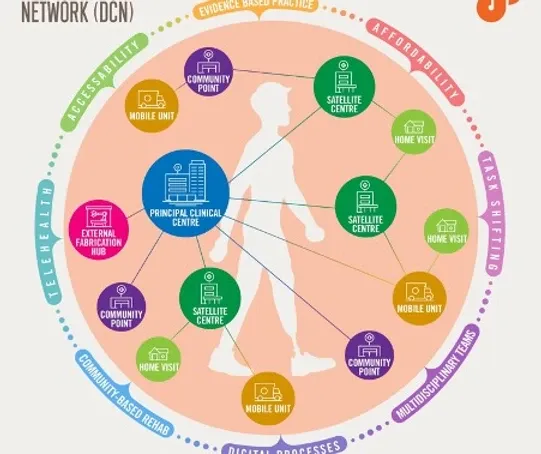
As we look to the future, the prosthetics industry stands on the cusp of a significant transformation, driven by the convergence of data-driven approaches and artificial intelligence (AI). Along with the new trends of a more proactive and remote healthcare, the rise of AI technologies presents an unprecedented opportunity to overcome many of the traditional barriers that have hindered rapid innovation in this field.

AI’s capacity to process and analyse vast amounts of complex, multidimensional data could revolutionize how we approach prosthetic design, fitting, and optimization. Machine learning algorithms can identify subtle patterns and correlations in user data that human analysts might miss, potentially leading to breakthroughs in prosthetic functionality and comfort. AI-powered systems could also help standardize and interpret the complex outcome measures inherent to prosthetics, making it easier to compare and evaluate different solutions across diverse user populations.
Moreover, the integration of AI with Internet of Things (IoT) technologies in smart prosthetics could dramatically increase the volume and quality of real-time usage data available for analysis. This wealth of data, when processed through sophisticated AI models, could enable truly personalized prosthetic solutions that adapt in real-time to users’ needs and changing conditions.
The application of AI in regulatory compliance and data privacy could also help address some of the legal and ethical challenges that have slowed innovation. AI systems could assist in anonymizing sensitive data, ensuring compliance with privacy regulations while still allowing for valuable insights to be extracted.
As AI technologies become more accessible and user-friendly, we can expect to see a democratization of data analysis capabilities within the prosthetics industry. This could help bridge the technical expertise gap, allowing a broader range of professionals to engage in data-driven research and development.
Furthermore, AI’s potential to accelerate the pace of research and development in prosthetics is immense. By automating many aspects of the design and testing process, AI could significantly reduce the time and resources required to bring new prosthetic innovations from concept to market. This acceleration could lead to a virtuous cycle where faster innovation attracts more investment and talent to the field, further driving progress.
In conclusion, while the prosthetics industry has faced numerous challenges in adopting data-driven approaches, the rise of AI presents a transformative opportunity. As these technologies mature and become more integrated into the prosthetics ecosystem, we can anticipate an exponential increase in the pace of data-driven research and development. This shift has the potential to usher in a new era of prosthetic technology, characterized by highly personalized, adaptive, and effective solutions that significantly improve the quality of life for users worldwide. The coming years are likely to witness unprecedented advancements in prosthetics, driven by the powerful combination of comprehensive data analysis and artificial intelligence.
This is the first in a series of blogs sponsored by the Douglas Bader Foundation looking at the current challenges and opportunities that lives of amputees. They will be used as a briefing papers for an international workshop.